Around 3 million Americans have some form of inflammatory bowel disease (IBD). IBD is used as a collective term to describe a group of chronic inflammatory diseases of the intestinal tract.
In most cases, IBD is diagnosed between the ages of 15 and 30. It is crucial to have a clear understanding of the various types of IBD, common symptoms, and appropriate management strategies. Understanding IBD can help you recognize the condition and seek medical care for its management.
Types of Inflammatory Bowel Diseases
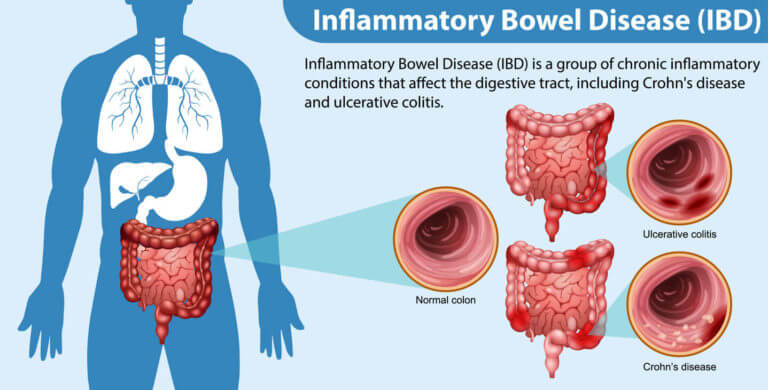
IBD is an autoimmune disorder, which causes the body to attack its healthy tissues and organs. The conditions under IBD cause inflammation, or pain and swelling, in the intestinal tract. Types of IBD include:
- Crohn’s disease – commonly affects the small intestine and the upper part of the large intestine.
- Ulcerative colitis – causes ulcers and swelling in the colon and rectum.
- Microscopic colitis – inflammation in the colon that requires the use of a microscope for diagnosis.
- Indeterminate colitis inflammatory bowel disease – a type of IBD that has both symptoms of Crohn’s disease and ulcerative colitis.
Many factors can increase your risk for IBD, including genetics and family history. About 1 in 4 people who have IBD have a family history of the autoimmune disease. However, it can also develop even if you do not have anyone in your family who has had IBD.
Other factors include the way your immune system responds to infections, the balance of bacteria in the gut, and environmental triggers such as stress or smoking.
Common Symptoms of IBD
Dealing with IBD is an individualized journey that varies from person to person. Some symptoms can range from mild to severe. Periods of severity in symptoms, also called IBD flareups, can vary over time.
Symptoms of IBD may include:
- Diarrhea (in some cases with blood)
- Constipation
- Gas and bloating
- Abdominal pain
- Unexplained weight loss or loss of appetite
- Fever
- Anemia
- Anxiety and depression
Rare symptoms of IBD may include vision problems, skin rashes, joint pain, and vomiting. Not all symptoms may be present in every case of IBD. When symptoms related to IBD are no longer present, it is referred to as being in remission.
Diagnosis and Management of IBD
To diagnose IBD, your healthcare provider will examine your medical history and will ask about which symptoms you are experiencing. They will also conduct a physical examination. Laboratory tests such as a complete blood count and stool test can also be employed during diagnosis to check for signs of inflammation. Imaging and diagnostic tests such as colonoscopy and a CT scan can help check for signs of IBD in your intestinal tract.
IBD treatments vary depending on the severity of symptoms and type. Various medications can help control the inflammation of the intestines, such as:
- Antibiotics – can treat abscesses and infections in the intestinal tract
- Aminosalicylates – anti-inflammatory medicine, such as mesalamine, sulfasalazine, or balsalazide
- Corticosteroids – help manage IBD flareups
- Immunosuppressants for IBD – drugs that suppress the immune system’s response to the intestine
- Topical anti-inflammatory medications – suppositories or enemas that can reduce diarrhea for mild to moderate IBD
Surgery for IBD
When medications are no longer effective in providing pain relief, surgery may be considered as an option, particularly for patients diagnosed with Crohn’s disease. Your surgeon will perform a bowel resection, during which they will remove the diseased segment of the intestine and connect the two ends of the healthy bowel in a process called anastomosis.
For patients with ulcerative colitis, your surgeon may perform a colectomy to remove the colon or a proctocolectomy to remove both the colon and rectum. Afterward, they connect the small intestine and anus, and then create an ileal pouch, which collects stool. An ileostomy may be done depending on the patient’s IBD case.
Lifestyle Changes for IBD
Eating certain foods may cause improvement for people who have IBD. A diet high in omega-3 fatty acids, which is found in oily fish and flax seeds, can ease intestinal inflammation. A low-residue fiber diet can also be helpful for patients with narrowed bowels due to IBD to reduce bowel irritation.
Dairy products such as milk and cheese may also trigger IBD flareups. Generally, keeping a food diary can help you keep track of your reaction to certain foods and help you understand which foods comprise the best diet.
Other lifestyle changes you can do to help manage IBD are adhering to a good sleep schedule, avoiding dehydration, and finding ways to manage stress. Some patients diagnosed with IBD find joining support groups beneficial in managing their condition.
Gastroenterology Services in New Jersey
While IBD is a lifelong condition, it does not need to shorten or limit your life expectancy. There are many ways to manage this condition, which could lead to long periods of remission and reduced IBD flareups. Early diagnosis and proper management of IBD are vital in making sure your IBD doesn’t get in the way of you living your best life.
Here at the Hudson MD Group, our multi-disciplinary medical practice encompasses a variety of quality healthcare services available to patients living in the New Jersey area. We provide expert patient care dedicated to getting you primary and specialty care.
Seek medical attention today if you think you are experiencing inflammatory bowel disease (IBD). If you or a loved one are experiencing symptoms of IBD, call our friendly offices and schedule an appointment today at (973) 705-4914.
We look forward to serving you!


